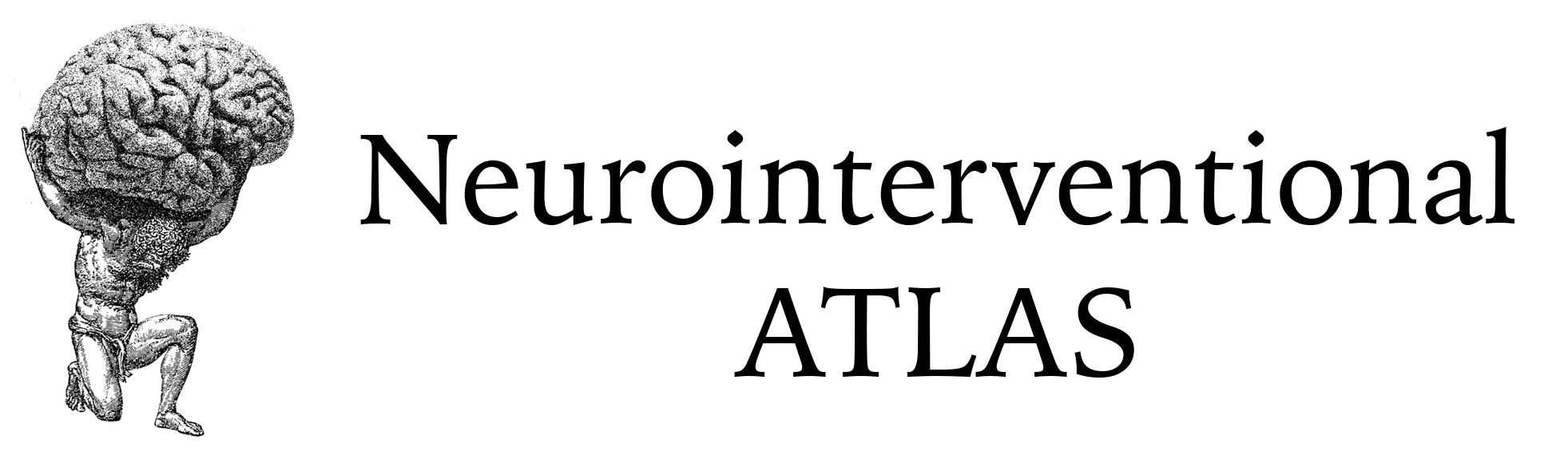
This is a case of an upper 90s-year-old patient who presented to the hospital with a T12 compression fracture and intractable pain localized to the region of interest.
A CT of the thoracic spine demonstrated a compression fracture of the T12 vertebral body with 50% vertebral body height loss and 4 mm bony retropulsion:
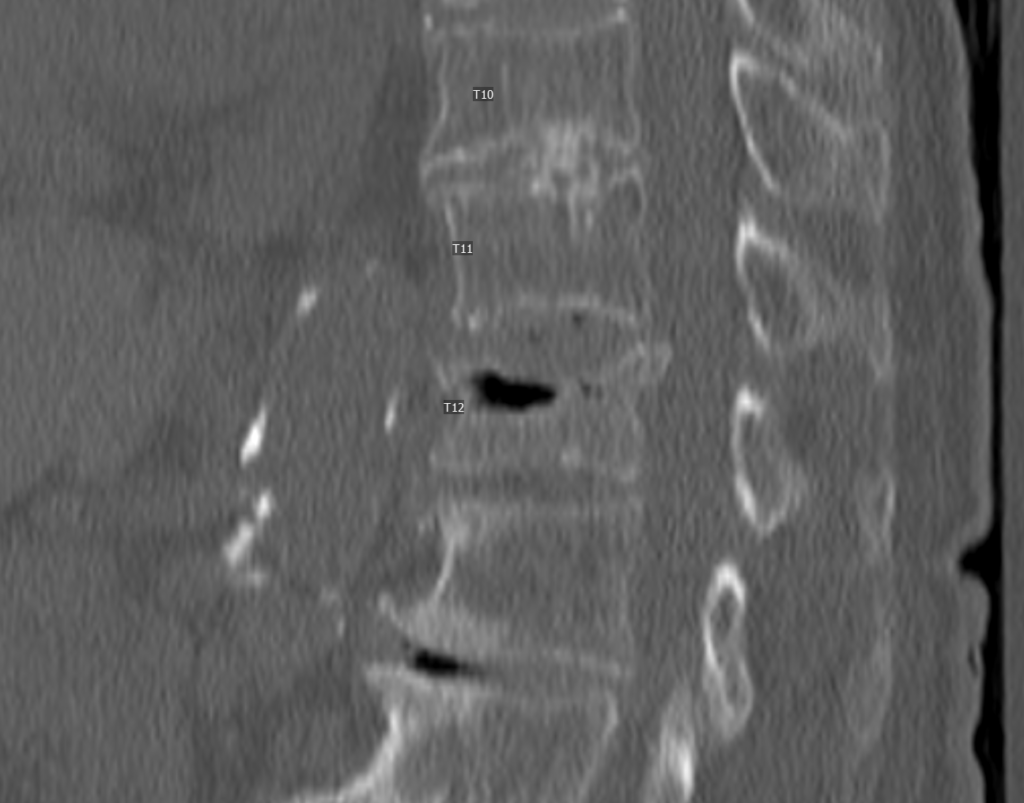
The decision was made to proceed with vertebroplasty following an informed discussion with the patient and family. The patient was managed with MAC by anesthesia.
Using the ringed forceps, the planned entry point of the right T12 pedicle was determined, and 1% bupivacaine was then infused subcutaneously as periosteally. Next, a small stab incision was made at the entry point, and the trocar and stylet were advanced through the subcutaneous tissue along this trajectory. The trocar and stylet were advanced to the posterior one third of the vertebral body using a combination of the entry view as well as the progress view.
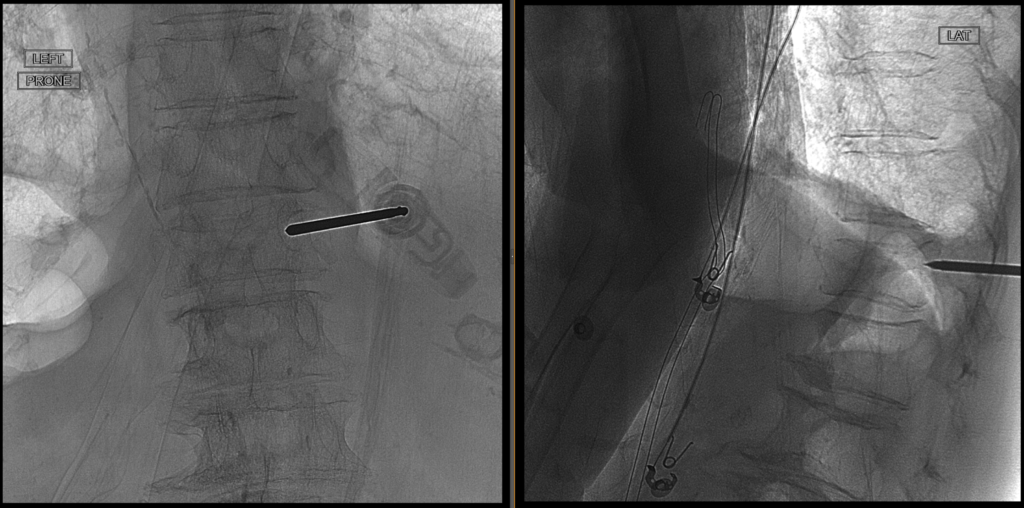
We then removed the inner stylet and replaced it with a curved stylet needle. This was advanced through the trocar in a curvilinear fashion. The final position of the curved stylet was on the contralateral side along the anterior one third of the vertebral body.
Next, the bone cement was mixed to adequate consistency, and then sequentially filled under fluoroscopic guidance.
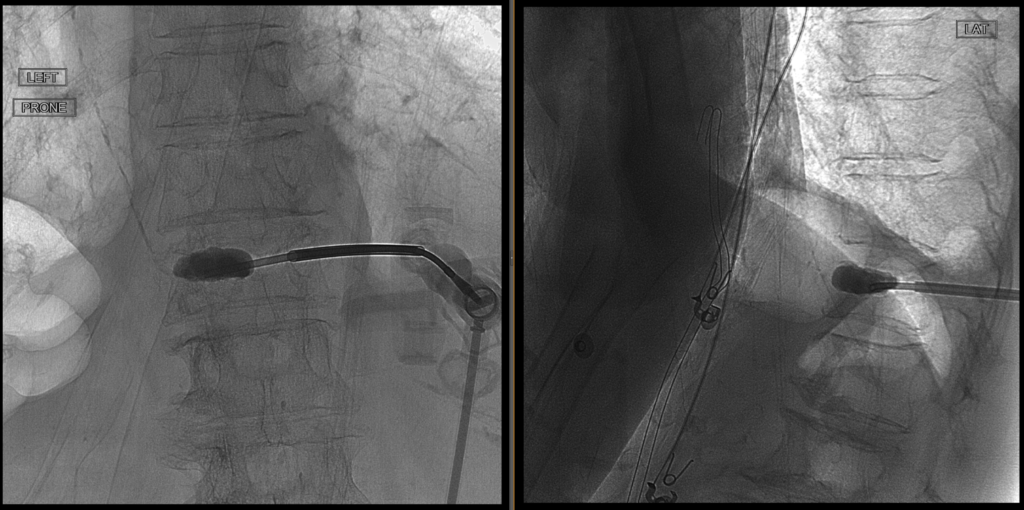
Here is the final view of the methyl methacrylate bone cement on AP View:

After adequate penetration of the bone cement was achieved, the curved stylet and trocars were removed. Hemostasis was obtained by manual pressure.
Following the vertebroplasty procedure, the patient experienced immediate pain relief and no longer required opioid pain medication. She was discharged safely home.